By Erin Zablocki, CDME, Master C.E.A.C., ECHM
Executive Director of Rehab Technology
ATF Medical
March is Brain Injury Awareness Month, and the Brain Injury Association of America’s tagline #MoreThanMyBrainInjury reminds us that someone with a brain injury is a person first. While a patient-centric approach should apply to all workers’ compensation patients, brain injuries require extra attention and resources.
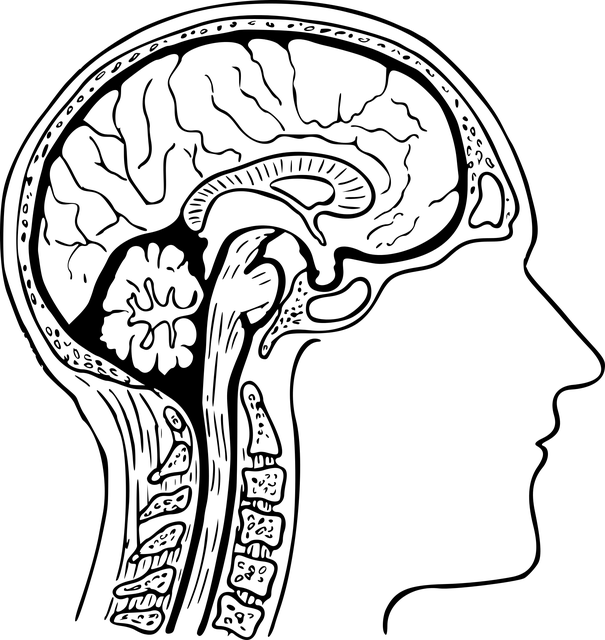
What exactly are brain injuries?
There are two overarching types of brain injuries: traumatic and acquired. Acquired or non-traumatic brain injuries alter the brain by internal factors. A lack of oxygen, exposure to toxins, pressure from tumors, and strokes are a few examples of the acquired types.
If an external force, such as being hit in the head, a fall, explosions, a gunshot wound or vehicular accident causes the brain injury, it’s a traumatic brain injury (TBI). These impact injuries can be open (penetrating) or closed.
The impact on workers’ compensation
Approximately 20% of work-related injuries of involve a TBI, according to the Centers for Disease Control and Prevention. TBIs are typically associated with high medical costs and long-term disability. The National Council on Compensation Insurance (NCCI) put the average cost of a claim involving a TBI at $84,000 in 2017. Medical inflation has pushed that number higher in the past five years. The industries most likely to incur brain injuries are construction, transportation and agriculture.
The impact of a brain injury on the patient
A brain injury cuts to the core of a person. It affects who the injured employee is—how they think, act, and feel.
Symptoms vary greatly from person to person, and no two brain injuries are exactly alike.
Brain damage can manifest in functional issues, such as physical weakness and a lack of coordination in the limbs. Visual impairment can be a symptom, and a brain injury can affect mobility and limit a person’s independence.
Cognitive effects, including confusion, memory loss, poor organizational skills, and poor reasoning skills are other symptoms. Patients tend to have trouble sleeping and suffer from fatigue.
They can be emotional, given to tears and anger. They may a lack impulse control and anger management abilities. Many patients are depressed, anxious and feel vulnerable and isolated. (Feelings of isolation are likely more prevalent with injured workers than other patients because they suddenly lose contact with most of their colleagues along with the sense of purpose working provides.)
Returning home after the injury
Injured employees with serious brain injuries receive hospital treatment and rehabilitation in a post-acute care center, preferably one that specialists in brain injuries. These facilities are highly structured and keep patients on busy schedules.
Heading home after living in such a regimented environment can be disconcerting. Suddenly, the injured person has to figure out how to live while dealing with the loss of some capabilities.
Naturally the home must be adapted to provide a safe and accessible environment. Ramps, roll-in showers, and door widening are typical home modifications. At the same time, rehab equipment, such as ceiling lifts, hospital beds, special mattresses, door openers, and wheelchairs are often required.
Payers need to determine what modifications and rehab technology will benefit a particular worker and not let the contractor or equipment providers go on autopilot. Clinically focused specialists, like occupational therapists, Certified Environmental Access Consultants, Assistive Technology Professionals and those holding Executive Certificates in Home Modification should collaborate with contractors to design an appropriate plan. The end product needs to accommodate the size and weight of equipment while fostering mobility, independence and functionality for a specific injured employee with specific symptoms and needs.
Communication among specialists, with the payer’s claim representatives, and especially the injured employee and their family are essential ingredients to delivering clinically appropriate solutions. The injured employee’s journey to recovery – or acceptance of their condition – is arduous enough. They and their families do not need the stress and frustration that comes with getting equipment they can’t use or not knowing when the construction crew will come or the powerchair will arrive.
Paying attention to the family
Family dynamics is a major psychosocial barrier to recovery. And adjusting to a new reality, and in some cases--a new personality--is hard on everyone, especially hard on family members living in the home.
Roles and boundaries may need to be re-negotiated, and schedule changes are a given. Home health caregivers will be introduced. Dealing with the patient’s mood swings, depression and anger drain spouses’ reserves. The day-to-day duties and constant vigilance wear down the most diligent caregivers. And divorce rates among seriously injured employees are high.
Families often benefit from professional psychological services and support groups. The BIA provides a list of virtual support groups, organized by states. Information can be found here Virtual Support Groups - Brain Injury Association of America (biausa.org).
Returning to work
The severity of the injury and the status of recovery determine if an employee can return to work after a brain injury. Some workers return to their previous positions with no problem and others can resume their roles with help from assistive technology and ergonomic adaptions and/or reduced responsibilities.
In other cases, flexible, hybrid, work-from-home, or part-time schedules are appropriate. Transferring to a different position in the organization or receiving vocational rehabilitation and seeking a different job are other routes to explore.
Employers and employees should have frank, empathetic, and open discussions about the person’s abilities and stamina and the workplace environment as they select the best option.
Summary
Living with a brain injury calls for a wide range of resources and strategies. The people who manage their claims and providers who care for them need to be empathetic. And they need to advocate for the best home and work environment possible.
# # #
Bio
Erin Zablocki, CDME, Master C.E.A.C., ECHM
Executive Director, Rehab Technology
ATF Medical
As Executive Director of Rehab Technology for ATF Medical, Erin Zablocki leads skilled teams of complex rehab equipment and adaptive housing coordinators as well as rehabilitation technology specialists.
She has more than 17 years of experience with complex rehabilitation and home modifications. With much of that experience in workers’ compensation, Zablocki has mastered the art of balancing the needs of injured workers against the cost-containment requirements of insurers, employers and third-party administrators.
Her experience includes overseeing catastrophic cases, providing equipment recommendations, and managing home modifications for a large national third-party administrator. Previous employers include Total Mobility Services and Total Medical Solutions.
In addition, Zablocki has volunteered as a Disaster Action Team Lead for the American Red Cross since 2020.
She holds the designations of Certified DME Specialist (CDME), Master Certified Environmental Access Consultant (CEAC), and Executive Certificate in Home Modifications (ECHM) through the University of Southern California, and is a Medicare Set-Aside Professional, trained through the University of Florida in Gainesville, Florida.