Share This Article:
Charleston, WV (WorkersCompensation.com) -- Whether medication is necessary is a medical decision, but for workers' compensation purposes, it is also a legal question, often with a court having the final say.
For example, in Becca v. Eagle Manufacturing, No. 21-0855 (W.Va. 09/14/23), although a worker's doctor advised that the worker needed opioids and medication to deal with their side effects, the court had different ideas.
The laborer injured her left wrist and arm when a block of material fell backwards and hyperextended it. More than two years later, an independent medical evaluation concluded that the laborer had reached maximum medical improvement and opined that no further treatment or testing would improve her condition.
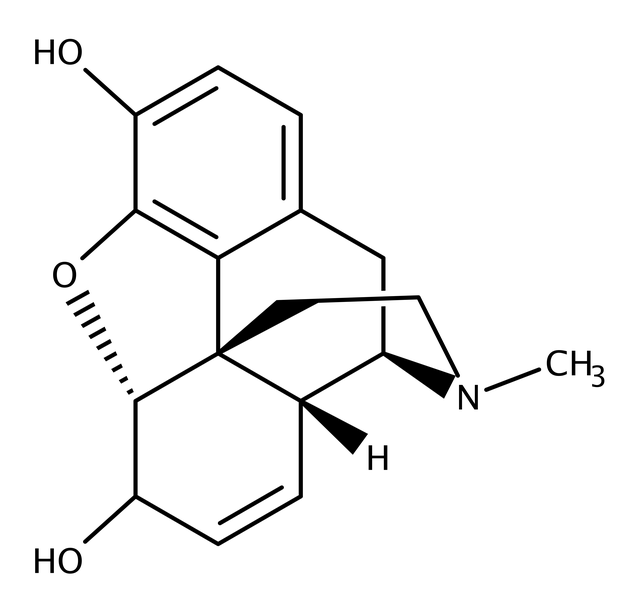
Eventually, the laborer's doctor requested authorization for Movantik, Norco, Xtampza, and Narcan for diagnoses of chronic low back pain and chronic pain syndrome. A peer reviewer requested by the claims administrator opined that the requested medications should not be for the following reasons:
--> Movantik is a second-line treatment for constipation related to opioid use, and there was no indication that the laborer failed first-line medication treatment.
--> Regarding Norco and Xtampza, the peer reviewed noted that state law requires documentation of: 1) meaningful pain relief; 2) functional benefits; and 3) an evaluation for compliance before such medications may be authorized.
Additionally, the doctor's request for Narcan, a first-line rescue for opioid overdose, was denied because the request for opioids wasn't supported by the evidence.
Eventually, the Office of Judges affirmed the claims administrator's denial of authorizations of the medications, finding that there was no indication that the lower back or chronic pain syndrome were compensable.
The laborer appealed to West Virginia's highest court.
In West Virginia, when a requested medication is an opioid, state law provides that the attending physician must, within 30 days, submit a written report that includes:
(1) A treatment plan with time-limited goals, including a time schedule to wean the injured worker from opioid use.
(2) A consideration of the prior medical history.
(3) A summary of conservative care rendered to the worker that focused on the reactivation and return to work.
(4) A statement on why prior or alternative conservative measures may have failed or are not appropriate as sole treatment.
(5) A summary of any consultations that have been obtained,
particularly those that have addressed factors that may be barriers to
recovery.
(6) A statement that the attending physician has concluded appropriate screening.
(7) A statement that the attending physician has conducted
appropriate screening for factors that may significantly increase the
risk of adverse outcomes (e.g., a history of addiction).
(8) An opioid treatment agreement that has been signed by the worker
and the attending physician. This agreement must be renewed every six months. The treatment agreement must outline the risks and benefits of opioid use, the conditions under which opioids will be prescribed, the physician's need to document overall improvement in pain and function, and the worker's responsibilities.
Additionally, when treating with opioids, the attending physician must submit the following every 60 days:
(1) Documentation of drug screenings, consultations, and all other treatment trials.
(2) Documentation of outcomes and responses, including pain intensity and functional levels.
(3) Any modification to the treatment plan.
Affirming the Office of Judge's ruling, the court held that the laborer failed to show that the requested medications were necessary treatment for her compensable injury.
"The medications Norco and Xtampza are opioids and ongoing authorization of such medications requires extensive documentation including a treatment plan, a weaning plan, regular drug screenings, and statements from physicians," the court wrote. "[The laborer] provided no such documentation."
Without authorization for opioids, the medications that were requested to treat side-effects of routine opioid use were also properly denied.

AI california case file caselaw case management case management focus claims compensability compliance compliance corner courts covid do you know the rule employers exclusive remedy florida glossary check Healthcare hr homeroom insurance insurers iowa leadership medical NCCI new jersey new york ohio pennsylvania roadmap Safety safety at work state info tech technology violence WDYT west virginia what do you think women's history women's history month workers' comp 101 workers' recovery Workplace Safety Workplace Violence
Read Also
About The Author
About The Author
-
Frank Ferreri
Frank Ferreri, M.A., J.D. covers workers' compensation legal issues. He has published books, articles, and other material on multiple areas of employment, insurance, and disability law. Frank received his master's degree from the University of South Florida and juris doctor from the University of Florida Levin College of Law. Frank encourages everyone to consider helping out the Kind Souls Foundation and Kids' Chance of America.
More by This Author
- Jan 02, 2026
- Frank Ferreri
- Jan 01, 2026
- Frank Ferreri
Read More
- Jan 04, 2026
- Liz Carey
- Jan 03, 2026
- Liz Carey
- Jan 02, 2026
- Chris Parker
- Jan 02, 2026
- Frank Ferreri
- Jan 01, 2026
- Frank Ferreri
- Dec 30, 2025
- Chris Parker




